Your gynaecologist will ask about your family history as part of your pre-conception assessment. There are some conditions that run in families and lead to genetic problems. Some conditions suggest your baby may be at increased risk of a health problem.
The vast majority of babies are born healthy but a small number (2 to 3 in 100) have an abnormality at birth. Most of these abnormalities are classified as minor. This means that they don’t interfere with the baby’s physical health or intellectual ability. A small proportion of abnormalities are considered major. This is because they can impair the baby’s quality of life or may be linked with stillbirth or premature death.
Genetic Screening
Genetic problems in the unborn baby are very rare. Less than 1 in 500 pregnancies have genetic problems. But there are some conditions which make having a pregnancy affected by a genetic disorder more common.
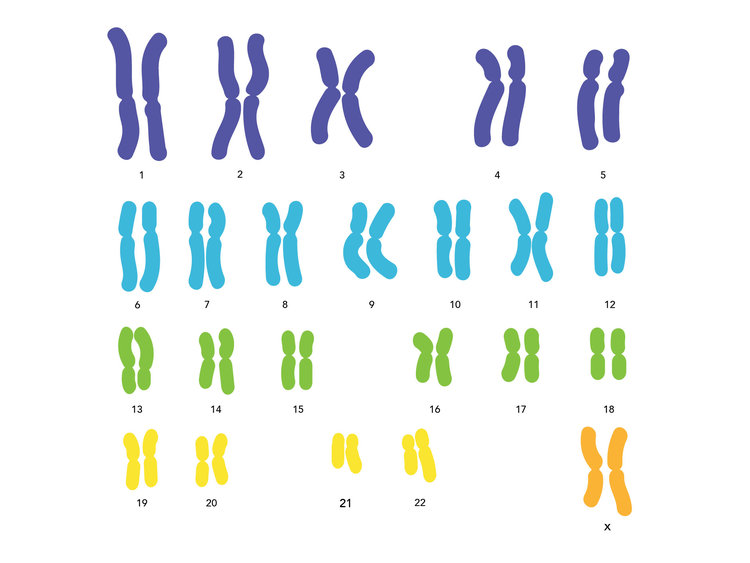
Older women (over the age of 36 years) have an increased risk of having a baby with three copies of a chromosome. Such as in conditions like Down syndrome (three copies of chromosome 21 as shown below). This might be a factor in your decision-making about when is the right time for you to start a family.
Miscarriages
Couples experiencing two or more miscarriages may have an underlying genetic problem. This may be in one or both parents and genetic testing of parental chromosomes may be indicated. Both partners should give as much information as possible to your gynaecologist about previous pregnancies. Regardless of the outcome of those pregnancies. Your information will be kept completely confidential and only disclosed with your consent.
Inherited conditions
If there is a family history of inherited conditions there may be an increased risk to your pregnancy. So please give as much family history to your gynaecologist as you can.
You will be offered screening for conditions such as sickle cell disease and thalassaemia. These are known as haemoglobinopathies. These conditions usually cause no or very mild symptoms in carriers. But if a child inherits the abnormal haemoglobin gene from both parents, they can suffer from serious blood disorders.
There are other rare genetic disorders such as cystic fibrosis. These only cause problems if a baby inherits the abnormal gene from both parents. It is now possible to screen for some of these conditions.
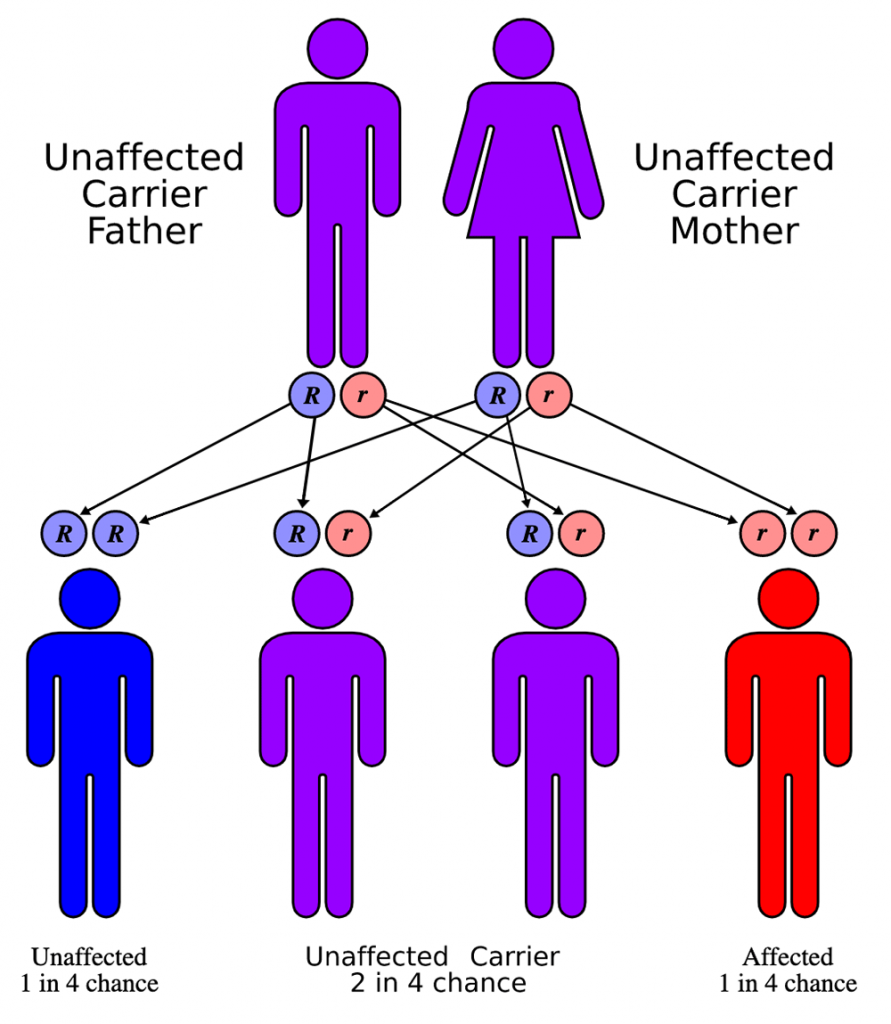
The woman has a blood test to look for the abnormal gene and if one is detected, then her partner is also screened. In the very rare situation of both of the couple carrying the same abnormal gene, the baby has a 1 in 4 (25%) chance of being affected. In this rare (but serious) situation, an affected pregnancy can be avoided by a specific type of IVF treatment called pre-implantation diagnosis. Your gynaecologist can explain this to you in more detail if it’s relevant to you.
The law in Cayman.
It is important to remember that termination of pregnancy is against the law in the Cayman Islands.
Ask your gynaecologist for more information about screening for anomalies in pregnancy.
More Advice on Genetic Problems
It’s also worth checking out help, advice and any genetic problems posts in our Baby Facebook Group. It allows you to ask questions, gain access to basic advice and share experiences with others facing the same new experiences. You can join here: https://www.facebook.com/groups/babycayman/

